Corneal Cross-Linking
for St. Petersburg & Clearwater, FL
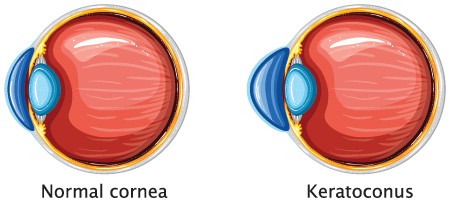
The cornea is the “window” at the front of your eye that helps focus incoming light for clear vision. Collagen is an essential protein that holds the cornea together. Collagen fibers form strong chemical bonds with nearby structures in the cornea, and when these links are weakened by disease or injury, the cornea warps and bulges. Vision abnormalities such as blurred vision, double vision and even vision loss can occur, but collagen crosslinking stiffens the cornea to reduce the bulging shape and preserve your eyesight.
Patient Education Video
Collagen Crosslinking Candidates
Our Ophthalmologists at St. Michael’s Eye & Laser Institute in Largo perform collagen crosslinking for patients with keratoconus or ectasia after LASIK, both rare. Keratoconus typically affects people between the ages of 10 and 25. The disease causes corneal thinning that slowly changes your cornea’s smooth, round contour to a bulging cone-like shape. Contact lenses or prescription glasses may improve your vision, but corneal crosslinking or corneal transplant surgery may be necessary in some cases to prevent vision loss. Collagen crosslinking is the standard of care for keratoconus worldwide.
Keratoconus symptoms include:
- Light sensitivity
- Double images
- Blurry vision
- Distorted images
- Difficulty seeing in low light environments
- Vision loss
Ectasia is a rare LASIK complication. The LASIK procedure creates a flap using the outermost layer (epithelium) of your cornea, which folds back for the laser to reshape the surface. The flap is placed back when the laser is finished, but the tissue removal sometimes weakens the cornea and leads to a cone-like bulge like keratoconus.
Collagen crosslinking can reinforce and strengthen the fibers in your cornea to prevent worsening symptoms.

Corneal Crosslinking Procedure Details
Collagen crosslinking “links” new fibers together in the cornea to stiffen the structure to stall or prevent the progression of keratoconus or ectasia and preserve your remaining vision. The FDA-approved procedure is minimally invasive and begins with numbing drops. A thin layer of the epithelium is removed to ensure maximum absorption of riboflavin eye drops (Vitamin B12), which are then applied continuously for 30 minutes. One of our Ophthalmologists will evaluate the progress to make sure enough riboflavin is absorbed by your eye(s).
A specialized device shines a focused beam of UV light rays at the cornea for an additional 30 minutes. UV light activates the riboflavin and promotes new bonds between the collagen fibers in the cornea. Collagen cross-linking takes about an hour in the surgical suite. A lens placed over the treated eye(s) for a week acts as a bandage while you heal.

Corneal Crosslinking Recovery
You may have some discomfort such as burning, itching or stinging in the eye for a few days after your procedure. You’ll be given prescription eye drops to use for several weeks. These will help ease any pain or discomfort you experience, and the bandage contact lens will help during your recovery too. Blurry vision is expected for several days and will improve around a week after removing the bandage lens.
Don’t touch or rub your eyes, keep water away from the eyes and avoid eye makeup and smoky or dusty environments. Most people who have collagen cross-linking for keratoconus or ectasia can return to work and drive within the first week of .
When you’ve healed fully, our Ophthalmologists will refit you for glasses or contact lenses.
Collagen crosslinking does not restore your vision or contour the cornea. The goal is to prevent the condition from worsening and avoid a more invasive procedure such as a cornea transplant.
Corneal Cross-Linking Results
Corneal cross-linking cannot cure keratoconus, but it is very effective at stopping or dramatically slowing the progression of keratoconus. Rather than restoring a normal corneal shape, cross-linking prevents additional vision loss by blocking keratoconus from progressing. This treatment is successful for over 90% of patients, and the results should last indefinitely. The sooner corneal cross-linking is performed, the better it can preserve vision.
Most patients only require treatment once to lock in their results, although it is possible to repeat the procedure months later if keratoconus continues to progress significantly.
Corneal Cross-Linking Costs
Corneal cross-linking cannot cure keratoconus, but it is very effective at stopping or dramatically slowing the progression of keratoconus. Rather than restoring a normal corneal shape, cross-linking prevents additional vision loss by blocking keratoconus from progressing. This treatment is successful for over 90% of patients, and the results should last indefinitely. The sooner corneal cross-linking is performed, the better it can preserve vision.
Most patients only require treatment once to lock in their results, although it is possible to repeat the procedure months later if keratoconus continues to progress significantly.
Fortunately, treatment for keratoconus — including corneal cross-linking — is covered by most health insurance plans. Your out-of-pocket costs will depend on your specific policy. Our team will submit claims to try to maximize the benefits you are entitled to. Financing options are also available.
Alternative Keratoconus Treatments
Corneal-cross linking is such an easy and effective treatment for keratoconus that it is the preferred method for most patients and Ophthalmologists when possible. Complementary treatments like Intacs, which are small inserts placed on the cornea to help flatten the curvature and improve vision, may be necessary depending on how far keratoconus has progressed prior to corneal cross-linking.
In extreme situations where keratoconus has advanced significantly, patients may require keratoplasty (or corneal transplant). Fortunately, this is generally avoidable thanks to other advancements like corneal cross-linking.
Corneal Cross-Linking FAQs
What are my chances of getting keratoconus or ectasia?
Both conditions are rare. Research suggests that approximately 0.05% of the population develops keratoconus. The estimates for the percent of patients who develop ectasia after LASIK or PRK are as low as 0.04%.
Does corneal cross-linking hurt?

What are the risk factors for keratoconus?
Scientists believe that keratoconus is often hereditary. About 10% of people with keratoconus have a parent with the same condition. Other risk factors include frequently rubbing your eyes (it is a good idea to always avoid touching your eyes) and having medical conditions like asthma, Down syndrome, Marfan syndrome, and Ehlers-Dano syndrome.
Will I still have to wear glasses or special contact lenses after corneal cross-linking?
Your prescription is likely to stabilize at the time you have CXL treatment. That means whatever prescription lenses you were wearing to see clearly just prior to your procedure will likely still be necessary. However, unlike many patients with uncontrolled keratoconus, you most likely will not need to constantly update your prescription.
How can I prevent having ectasia after LASIK?
One of the reasons that some people are deemed unsuitable candidates for LASIK is that they have thin corneas. A thin cornea is more susceptible to weakening with laser correction surgery and then bulging into a cone-like shape. To seriously reduce your risk of developing this problem, go to an Ophthalmologist (like those at St. Michaels) who you can trust to assess your candidacy correctly.
Contact St. Michael’s Eye & Laser Institute
If you’ve been diagnosed with keratoconus or ectasia, contact St. Michael’s Eye & Laser Institute to discuss your treatment options with collagen cross-linking.
 Patient Portal
Patient Portal  Online Payment
Online Payment  Doctor Referral
Doctor Referral  Financing
Financing